Hearing Wrap Up: Pharmacy Benefit Managers Prioritize Their Pocketbooks Over Patient Care
Congress can work in a bipartisan fashion to address unchecked PBMs
WASHINGTON – Today, the House Committee on Oversight and Accountability held a hearing titled “The Role of Pharmacy Benefit Managers In Prescription Drug Markets Part I: Self-Interest Or Health Care?” At the hearing, members and witnesses highlighted how Pharmacy Benefit Managers (PBMs) have an oversized role in the pharmaceutical marketplace and push anticompetitive practices that undermine patient health and drive up the cost of prescription drugs. Both Republicans and Democrats stressed there must be greater transparency in the PBM industry and Congress must address PBMs’ harmful tactics. The Oversight Committee will continue to examine PBM practices to inform legislative solutions that can greatly benefit patients and reduce drug costs.
Key Takeaways:
PBMs engage in self-benefitting, anticompetitive tactics which increase costs for consumers and harm patient care.
- Dr. Miriam Atkins, Oncologist, Augusta Oncology Associates: “Unfortunately, the PBM preferred drug is often not the best drug for a patient but the most profitable drug for the PBM… Treatment delays, denials, and fueling drug costs is the PBM hell my patients and I live in every day. The top PBMs have such leverage that they do what they want.”
- Mr. Greg Baker, CEO, AffirmedRx: “Currently, a handful of large PBMs control up to 80% of the market in the U.S. This is problematic for every employer in the country. These PBMs are not constrained by any obligation to be transparent on their pricing or methodology… this problem is also costing taxpayers significantly since some of the biggest health plans in the country are run by local and state entities.”
- Kevin Duane, Owner, Panama Pharmacy: “The outsized role PBMs take in the pharmacy space has caused many problems for our patients and our practice. The three largest PBMs control 80 percent of the market today, which means patients are forced by PBMs into using a certain pharmacy, often one owned and operated by the PBM, or they may be forced to get their drugs through the mail even though they want a pharmacist face-to-face in their community. Patients and their doctors have virtually no say in what drugs are used, since the PBM essentially forces which drugs can be used – not because a drug is better or worse, but because the PBM can make more money from it.”
Greater transparency in the PBM industry is necessary to determine the impact PBM tactics are having on patients, the pharmaceutical market, and health care programs administered by the federal government.
- Mr. Greg Baker, CEO, AffirmedRx: “It is possible to operate a PBM, restrain costs for the employer and taxpayers while still providing the best pharmacy care available. But changes must be made to require greater transparency and allow for greater competition for this to happen.”
Congress has a responsibility to act. The Oversight Committee can work in a bipartisan fashion to shine a light on how PBMs undermine health practices, harm community pharmacies, and prioritize their pocketbooks over patients.
- Chairman James Comer (R-Ky.): “Congress has talked about this issue for a long time. But what I think you are going to see moving forward is actual action. It’s past time to do something about PBMs … We are sincere about identifying waste, fraud, and abuse in the federal government. And when you look at problems that every American has, prescription drug costs are at the top of the list.”
- Rep. Raja Krishnamoorthi (D-Ill.): “According to the government, these [Direct and Indirect Remuneration (DIR)] fees increased by 107,400 percent from 2010 to 2020. This is a travesty. You know what PBM really stands for? It stands for Pretty Big Markups. We’ve got to stop this… A recent poll by Morning Consult showed that in March 2023 that 85 percent of Americans are concerned that PBMs are overcharging for prescription medicines and pocketing the difference as profit. In that survey 88 percent of Democrats and 88 percent of Republicans shared that concern … I think we have a mandate from the American people to investigate.”
Member Highlights:
Committee Chairman James Comer (R-Ky.) emphasized that three large PBMs collectively control approximately 80 percent of the health market and engage in self-benefitting practices that boost their bottom line without a benefit to patients.
Chairman Comer: “Instead of fierce competition, three large PBMs—CVS Caremark, Express Scripts, and Optum Rx—collectively control approximately 80 percent of the market. Every major PBM is owned by a major health insurer and owns or is owned by a specialty, mail-order, or retail pharmacy, or all three. This means that when PBMs negotiate with a pharmacy or a health insurer, they are either negotiating with themselves or one of their direct competitors. Today, PBMs engage in self-benefitting practices that boost their bottom line without a benefit to patients.”
Chairman Comer stressed that PBMs’ anticompetitive tactics are driving up health care costs for Americans and harming patient care. He noted the importance of greater transparency in the PBM industry to combat their detrimental tactics that are harming patients, the pharmaceutical market, and health care programs administered by the federal government.
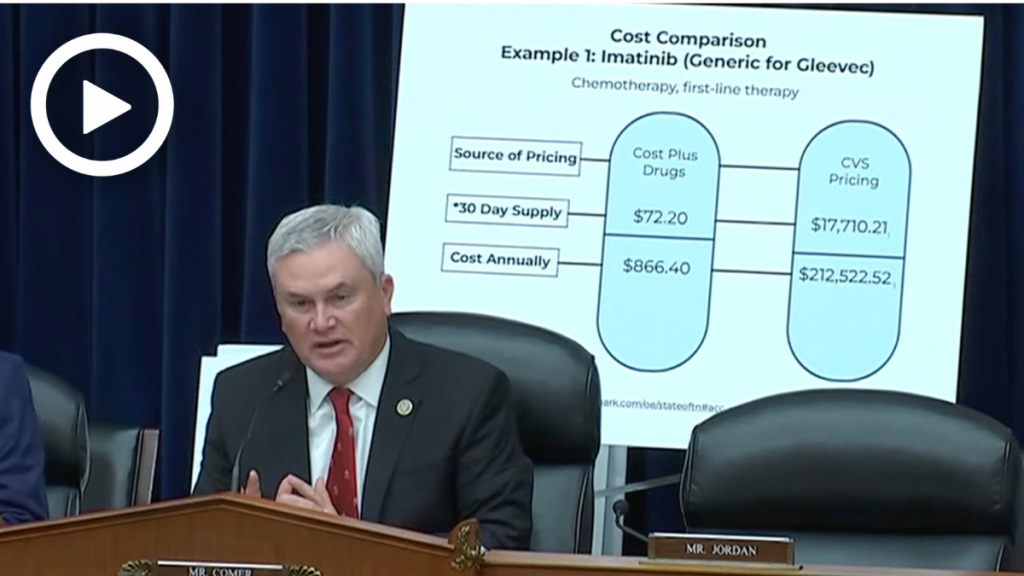
Chairman Comer: “Mr. Baker, you are the CEO of AffirmedRX, a PBM that works to promote transparency. AffirmedRX is the PMB for Mark Cuban’s company Cost Plus Drugs. I want to show the comparison between how much the drug would cost a patient if they bought it at Cost Plus Drugs versus if they got it at CVS. Imatinib, a generic chemotherapy drug, can cost a patient at CVS more than $17,000 for a 30-day supply. An identical prescription would only cost $72 at Cost Plus Drugs. That is a massive difference. Mr. Baker do you attribute the difference in cost to PBMs?”
Mr. Greg Baker: “I do.”
Chairman Comer: “Dr. Atkins, do you think a patient is more likely to take a cancer drug if a drug is $72 or $17,000?”
Dr. Atkins: “$72 for sure.”
Chairman Comer: “So would you agree that insane prices on vital medication like this are killing people?”
Dr. Atkins: “Yes.”
Rep. Virginia Foxx (R-N.C.) highlighted serious concerns over PBM industry policies that prevent or delay patients from accessing critical medicine they need. She stressed that we need transparency in the PBM industry and in the cost of medical care.
Rep. Foxx: “I have serious concerns over the PBM industries promotion of failed first policies that can prevent or delay patients from accessing medicine they need. Dr. Atkins in your role do you have patients required to ‘fail first’ on a medication and what can you do?”
Dr. Atkins: “We deal with fail first almost every day… We try to talk to the PBM. Sometimes that works and sometimes that doesn’t.
Rep. Foxx: “We need transparency. That is the whole issue… We need transparency in pricing. We must have transparency in the cost of medical care. We have the best care in the world, but it is also the most expensive.”
Rep. Andy Biggs (R-Ariz.) pointed out that deceitful tactics pushed by PBMs are driving prescription drug costs higher for all Americans, including the men and women who serve in the U.S. Armed Services.
Rep. Biggs: “Have PBMs made it more difficult for veterans and service members to access prescription drugs in a timely manner?”
Dr. Kevin Duane, Owner, Panama Pharmacy: “Absolutely…”
Rep Biggs: “I think we have created a PBM industry where the general mantra is in chaos, there is profit. This doesn’t help anyone. This is something we need to continue to work on and look at.”
Rep. Gary Palmer (R-Ala.) pointed out that PBMs are pocketing an exorbitant amount of money from the rising prices of prescription drugs. He emphasized that PBMs are engaging in self-benefitting pricing strategies and that the Committee can work in a bipartisan fashion to address unchecked PBMs.
Rep. Palmer: “PBMs act as middlemen… what I want to know is where is all this money going. Is it possible that PBMs are pocketing the difference? Because it is not getting back to the patient.”
Mr. Baker: “That would be my contention as well.”
Rep. Palmer: “I think this is extremely important… I think we can work in a bipartisan way to come up with solutions to help patients. We need to know where all these profits are landing.”
Rep. Pat Fallon (R-Texas) emphasized that 2,300 independent pharmacies have closed in the United States in just three years and rural communities are paying the price. He noted that a large PBM, Express Scripts, recently announced that they would be reducing prescription reimbursements for 10 million Tricare members and 15,000 rural pharmacies were dropped from the Tricare network.
Rep. Fallon: “In the Fall of 2022, Express Scripts announced they would be reducing prescription reimbursements for 10 million Tricare members. Additionally, 15,000 primarily rural and independent pharmacies were then dropped from the Tricare network. That is particularly concerning to me since I represent 10 rural counties… How does this impact access and competition? It was reported that Express Scripts removed rural staples like Walmart, Kroger, and Sams Club in favor of CVS, of course a pharmacy that is owned by one of the other Big 3. Do you find it harder to compete in the market?”
Mr. Baker: “We absolutely do.”
Rep. Fallon: “If we are removing competition from Tricare networks, how does that improve service and lower costs?”
Mr. Baker: “It does not do either of those things.”
Rep. Chuck Edwards (R-N.C.) highlighted that states around the country are also taking action to address rising drug costs and combat anticompetitive tactics pushed by PBMs.
Rep. Edwards: “What we did in the North Carolina legislature is we gave more authority to our insurance commissioners and provided tools to make PBMs more transparent and to regulate them. Have you seen any other state that has taken action?”
Dr. Duane: “States have taken steps. The state of Florida has passed a large bill to address a lot of the things… Other states have looked at pricing structures. What states are doing and how they are regulating have lowered some costs.”
Rep. Byron Donalds (R-Fla.) asked witnesses to clarify how Americans are suffering because of the actions of PBMs.
Rep. Donalds: “In your testimony, you described PBM’s as the monster in a nightmare. Do you care to elaborate?”
Dr. Duane: “My wife and I bought the local pharmacy with an SBA loan… What I hoped could be and can be a great opportunity for my community is in peril because of the things we have talked about today. It has been a whole lot tougher.”
Dr. Atkins: “I would agree. When I first became a physician, I could just focus on taking care of my patients. Now every day I fight a faceless corporation that doesn’t understand what I do and really doesn’t care. They try to tell me how to take care of my patients and tell me what drugs we can and cannot use… All of these things interfere with patient care and their quality of life.”
Rep. Tim Burchett (R-Tenn.) highlighted the benefits of independent pharmacies and noted that PBMs never negotiate on contracts and fees charged to local pharmacies.
Rep. Burchett: “Can you explain the benefits of independent pharmacies?
Dr. Duane: “We can be the center of a community. We are more than just providing medication for people… We can help on things that they can’t get into right away with their physicians.”
Rep. Burchett: “These pharmacies contract with PBMs… What impact did their rising fees have on the healthcare market?”
Dr. Duane: “Huge. Indescribable amount of chaos. We cannot adequately plan because of the amount of money that is taken back.”
Rep. Lisa McClain (R-Mich.) highlighted that PBMs were originally intended to negotiate and drive the cost of drugs down for patients but have now evolved into middlemen with an aim to manipulate drug costs for higher profits.
Rep. McClain: “There is a problem here that needs to be fixed. Doesn’t matter what side of the aisle you’re on. Now we can get down to the bottom of it to fix it… PBMs it seems have evolved into middlemen with an outsized role in the pharmaceutical marketplace operating behind the scenes to manipulate drug costs and access for their own benefit. What do we think the number one goal or priority should be?”
Mr. Baker: “We have used the word transparency here quite a bit.”
Rep. McClain: “Who would benefit from increased transparencies in the PBM world?”
Mr. Baker: “The American taxpayer would benefit greatly.”
READ MORE:
Comer: Pharmacy Benefit Managers Are Making Billions at the Expense of Patients and Taxpayers
CLICK HERE to watch the hearing.