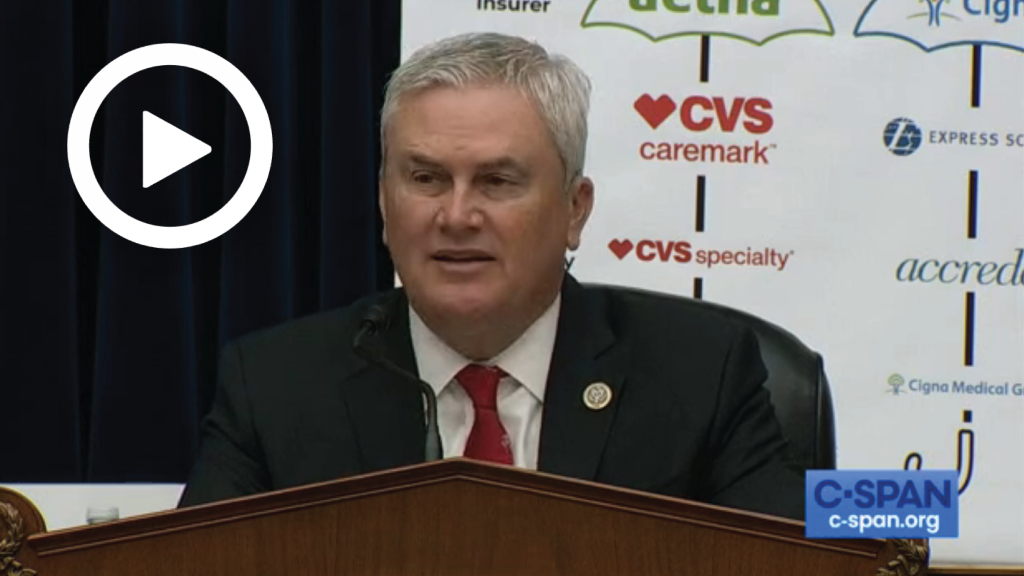
Comer: Pharmacy Benefit Managers Are Making Billions at the Expense of Patients and Taxpayers
WASHINGTON – Today, House Committee on Oversight and Accountability Chairman James Comer (R-Ky.) delivered opening remarks at a full committee hearing titled “The Role of Pharmacy Benefit Managers In Prescription Drug Markets Part I: Self-Interest Or Health Care?” In his opening statement, Chairman Comer emphasized that Americans are suffering from rising health care premiums and expensive prescription drug prices. He highlighted how Pharmacy Benefit Managers’ (PBMs) deliberate, anticompetitive tactics aim to prevent payers—including government payers like Medicare, Medicaid, TRICARE, and the Federal Employee Health Benefits program—from understanding how PBMs are making billions at the expense of patients and taxpayers. Today, three large PBMs collectively control approximately 80 percent of the health market and engage in self-benefitting practices that boost their bottom line without a benefit to patients. State legislatures across the country have passed legislation preventing some of their anticompetitive practices and Chairman Comer stressed that Congress also has a responsibility to act. In addition to the PBM Committee report released in 2021, Chairman Comer stressed that the Committee will press forward to shine a light on PBMs undermining health practices, harming community pharmacies, and prioritizing their pocketbooks over patients.
Below are Chairman Comer’s remarks as prepared for delivery.
Welcome to today’s hearing on the role of Pharmacy Benefit Managers in Pharmaceutical Markets.
Today, health care premiums have increased faster than inflation.
List prices for prescription drugs have gone through the roof even though net prices have declined.
And despite this increase in healthcare costs, life expectancy has remained stagnant.
That means someone is benefitting, and it isn’t patients.
Look no further than PBMs, or pharmacy benefit managers.
Today we will have our first opportunity to examine how the middlemen in the pharmaceutical supply chain impact the cost of prescription drugs for patients.
Today is the first public hearing this Committee had held to examine the behind-the-scenes tactics that PBMs use to prevent payers—including government payers like Medicare, Medicaid, TRICARE, and the Federal Employee Health Benefits program—from understanding how PBMs are making billions at the expense of patients and taxpayers.
When PBMs were first created, they were beneficial to the entire health care system.
There was more than a dozen large PBMs across the country, all competing with each other to provide clear details about costs, fees, and rebates to pharmacies and patients.
They were able to quickly tell pharmacists across the country whether insurance would cover a patient’s medication and what the patient’s copay would be.
They were able to negotiate reduced costs of prescription drugs, pitting competing manufacturers against one another.
They were able to drive down premiums for patients by encouraging greater adoption of lower cost medications.
But today they have largely outgrown this role.
Now, instead of fierce competition, three large PBMs—CVS Caremark, Express Scripts, and Optum Rx—collectively control approximately 80 percent of the market.
Today, every major PBM is owned by a major health insurer and owns or is owned by a specialty, mail-order, or retail pharmacy, or all three.
This means that when PBMs negotiate with a pharmacy or a health insurer, they are either negotiating with themselves or one of their direct competitors.
Today, PBMs engage in self-benefitting practices that boost their bottom line without a benefit to patients.
In the Medicare program, PBMs often claw back billions of dollars in reimbursements paid to competing pharmacies.
PBMs also steer patients to certain pharmacies and to certain medications.
By doing this, they can increase patients’ copays and force manufacturers to increase list prices in order to meet the PBMs’ higher rebate demands.
The big three PBMs have created group purchasing organizations, some incorporated abroad, to better hide the rebates and fees they receive.
It is hard to see how these tactics benefit patients.
State Attorneys General in Ohio, Oklahoma, Utah, Texas, and others have filed lawsuits and opened investigations into the anticompetitive practices of PBMs.
State legislatures across the country have passed legislation preventing some of their anticompetitive practices and requiring transparency in pricing and contracts.
The Federal Trade Commission opened an investigation into PBMs’ anticompetitive actions.
Congress must also act.
Last Congress, Oversight Republicans conducted a review of PBMs.
What we found was deeply concerning and raised many questions about PBMs’ role in the healthcare industry.
That is why the Committee is making examining PBMs a priority this Congress.
We hope to answer these questions:
How are PBMs using their position at the center of prescription drug markets to undermine patient health?
Why and how are PBMs using a system of hidden rebates and fees?
How are PBMs harming community pharmacies?
From what we have seen many PBMs are acting without consequence to the detriment of patients and their pocketbooks, because PBMs have been allowed to hide in the shadows.
It’s time to bring them into the light
###